2x Supartz Injections
Hyaluronic acid injection to help lubricate the ankle joint. Afterwards, mild irritation for ~1 day, but then pain-free for a couple weeks (so far) despite long periods of standing.

What Should He Do?
Hyaluronic acid injection to help lubricate the ankle joint. Afterwards, mild irritation for ~1 day, but then pain-free for a couple weeks (so far) despite long periods of standing.
Dr. Daniel Thuillier, MD — Foot and Ankle Surgery, UCSF Health
Download Full Report (PDF)Dr. Sagar Chawla, MD, MPH — Foot and Ankle Surgery, Cleveland Clinic
Third opinion from Dr. Danny Choung, DPM at San Rafael Podiatry.
Dr. Choung reviews the CT scan and explains the current state of the ankle:
MRI imaging of the left ankle.
Second opinion from podiatrist Dr. David Collman, comparing perspectives with Dr. Gentile's assessment.
Follow-up discussion on left ankle CT scan with Dr. Michael Gentile, DPM (Foot and Ankle Surgery).
Dr. Gentile reviews the CT scan and explains the current state of the graft:
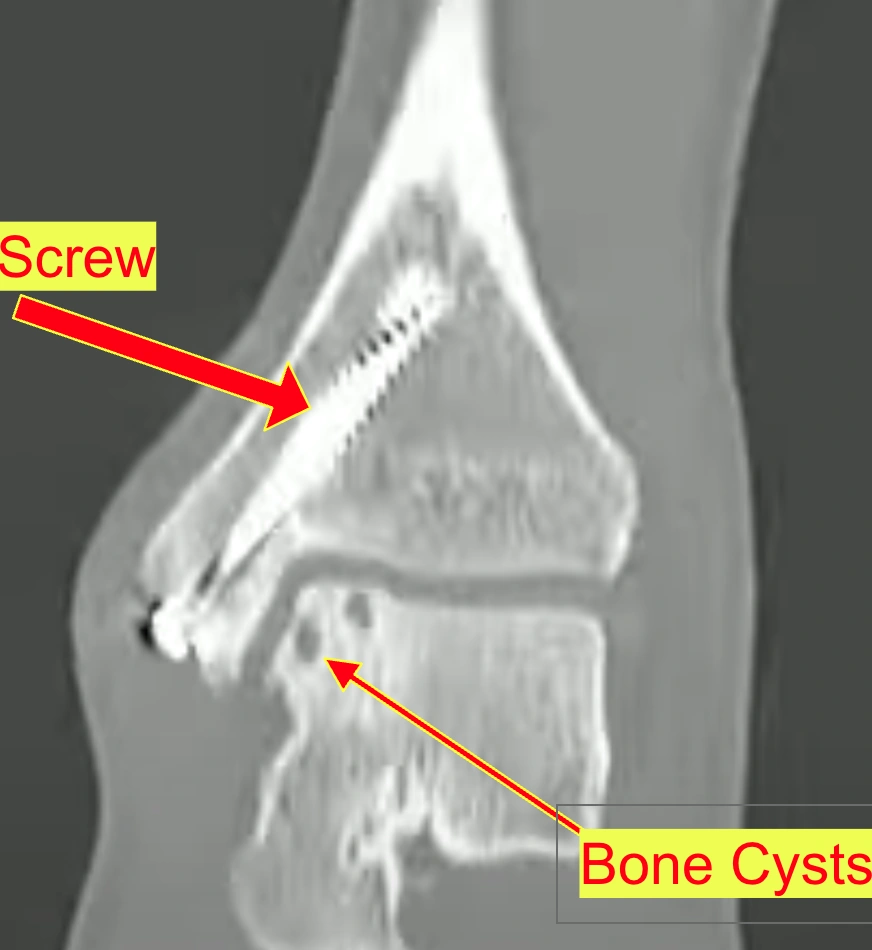
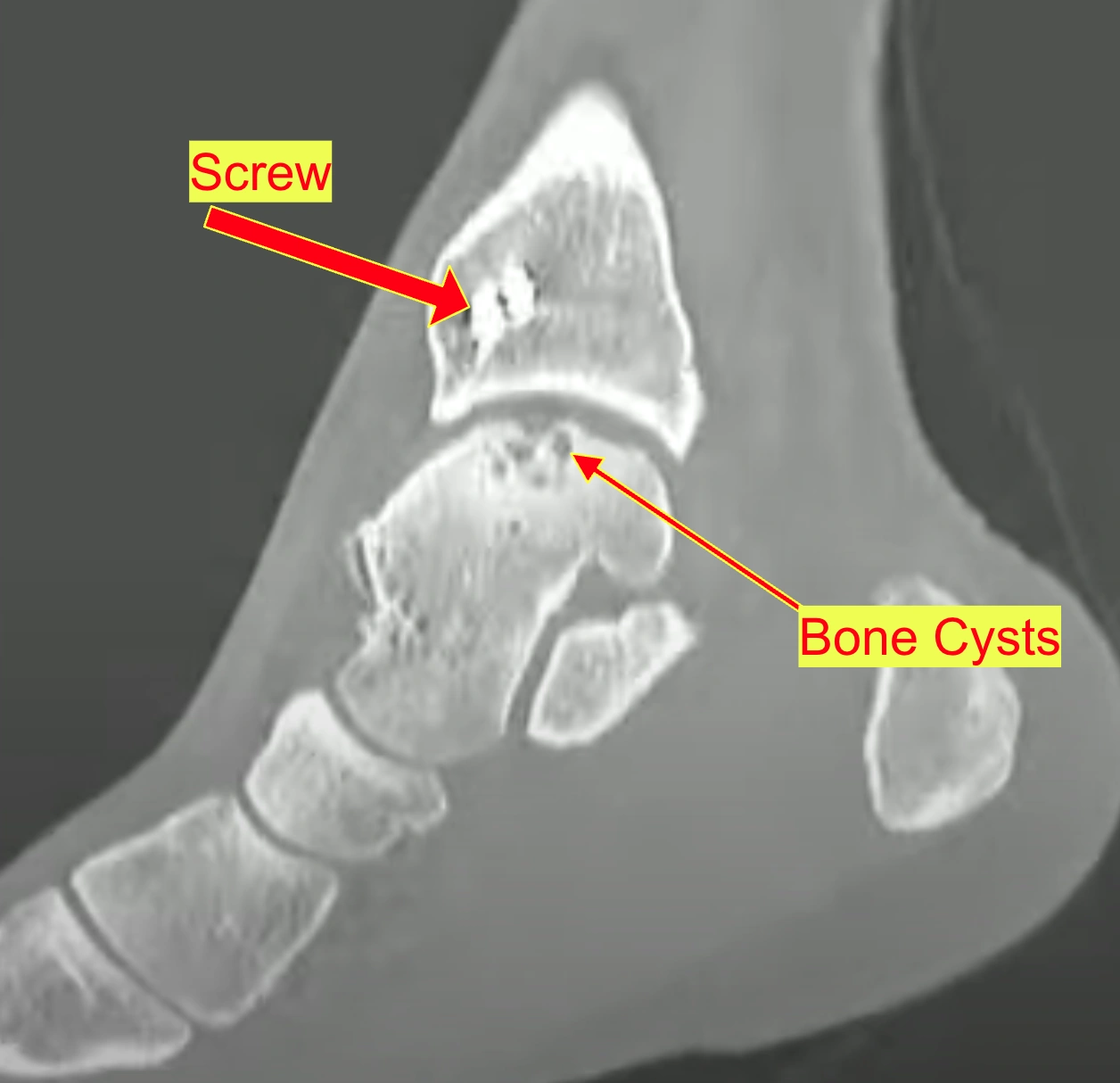
CT imaging of the left ankle. Compared with CTs from 9/27/2012 at Cayuga Medical Center.
Subcutaneous tissues and muscles are normal.
→ The skin, fat, and muscles around the ankle look healthy
No significant joint effusion. No calcified intra-articular bodies.
→ No swelling/fluid buildup in the joint, no loose bone chips floating around
Observed the return of dull ankle pain when standing for more than 1.5 hours in a day, or doing physical activity for more than 30 minutes.
No ankle pain. Played sports regularly with full range of motion and ankle strength.

Additional imaging to monitor ankle condition.

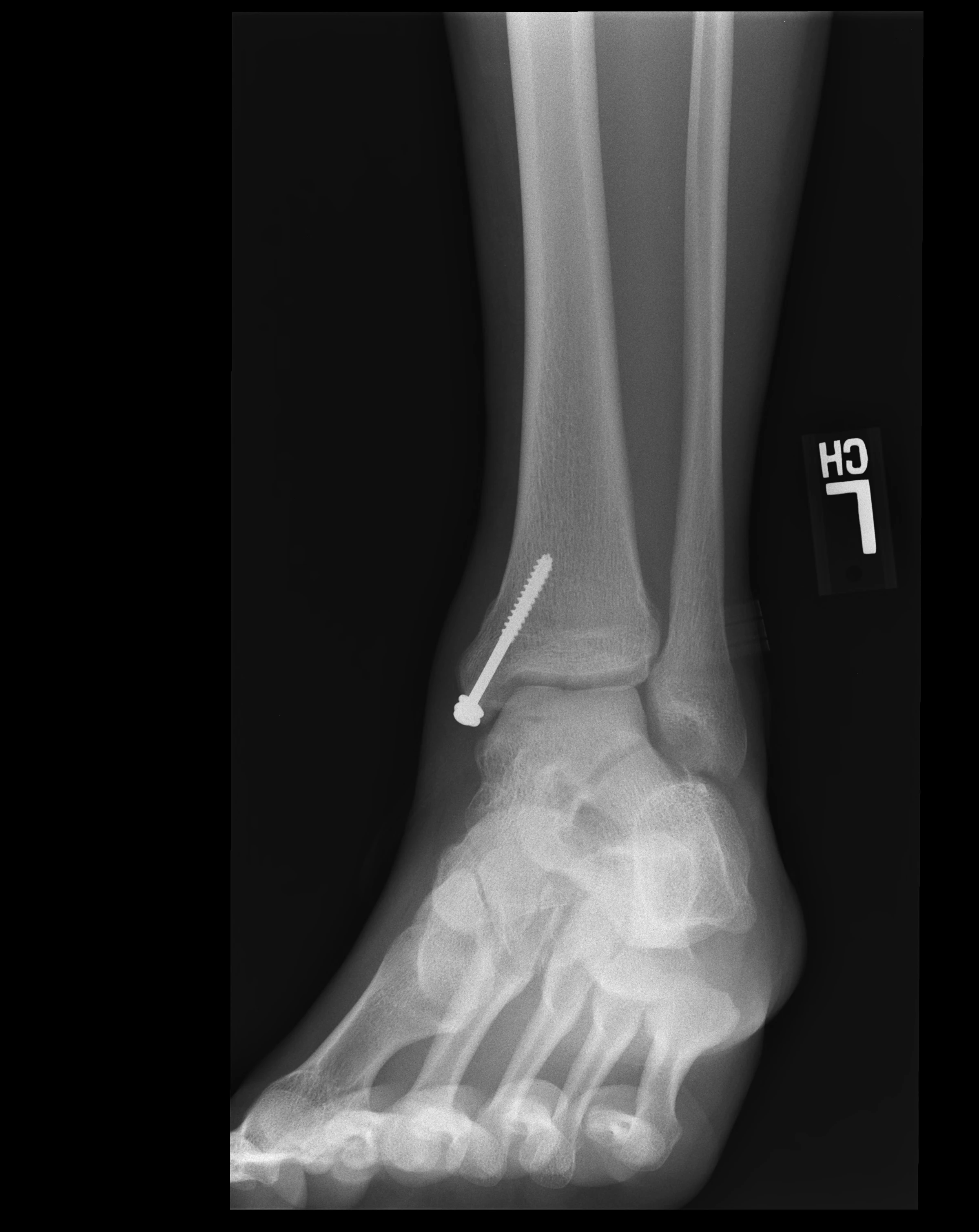
Post-operation imaging of the left ankle.
Diagnosed with an osteochondral lesion of the talus. The damaged bone and cartilage fragment needed to be removed, and the resulting defect would be filled with a talar osteochondral allograft (donor bone and cartilage transplant). Additionally, the ATFL (anterior talofibular ligament)—the ligament that prevents the ankle from rolling outward—would be tightened to restore stability.
CT imaging of the left ankle.

When standing for extended time, dull pain increases.
Initial CT imaging of the left ankle to assess the injury.
Over the following years, I sprained my ankle about 3 more times. Each sprain made the ankle floppier and easier to sprain again. By the last sprain, my ankle had become so loose that I sprained it just walking on grass.

Playing basketball at the local YMCA when it happened. There was some swelling, but the pain went away after about 2 minutes. No additional pain until the next sprain.

A comparison of recommendations from 5 different specialists consulted in 2025
Foot and Ankle Surgery (May 2025)
Podiatrist (August 2025)
San Rafael Podiatry (September 2025)
UCSF Health - Foot and Ankle Surgery (November 2025)
Cleveland Clinic - Foot and Ankle Surgery (November 2025)
| Option | Pros | Cons | Supported By |
|---|---|---|---|
| Conservative (HA Injections + Activity Modification) | No surgery, maintains options, low risk | Doesn't fix underlying problem, temporary relief | Choung, All doctors as alternative |
| Arthroscopy + Debridement | Minimally invasive, 2-week recovery, diagnostic value | May not help large lesions, doesn't restore cartilage | Collman, Cleveland Clinic |
| Arthroscopy + Bone Graft + BioCartilage | Restores bone, scaffold promotes healing | Newer technique, less long-term data | Cleveland Clinic |
| Repeat Osteochondral Allograft | Replaces damaged cartilage with healthy tissue | Higher failure rate for revisions, long recovery | Gentile, UCSF |
| Osteochondral Autograft (from knee) | Uses patient's own tissue, better integration | Donor site morbidity in knee, limited tissue | Choung (if surgery needed) |
A comprehensive analysis of current research on osteochondral lesions of the talus (OLT) with 144+ peer-reviewed sources covering all treatment options from conservative management to regenerative medicine (updated December 2025)
Osteochondral lesions of the talus involve damage to the articular cartilage and underlying bone of the talus (ankle bone). These lesions pose a therapeutic challenge due to the limited intrinsic healing capacity of cartilage and the talus's unique anatomical characteristics [1]:
The ankle is the second most frequent site, following the knee, that requires cartilage repair [5].
OLTs are generally classified as small or large based on:
A study in the American Journal of Sports Medicine identified 150 mm² as a critical cutoff for clinical failure. Only 10.5% of ankles with defects smaller than 150 mm² showed clinical failure, compared to significantly higher rates in larger lesions [6].
Raymond's lesion measures approximately 15mm x 10mm for cartilage loss and 15mm x 12mm x 10mm for the cystic bone component, placing it in the "large lesion" category.
Multiple studies have examined what happens when OLTs are not surgically treated:
→ MRI staging = how doctors classify OLT severity. Higher stages = more damage = likely need surgery. Lower stages may heal conservatively.
Several classification systems exist for staging OLT on imaging:
Hepple and colleagues revised the classification specifically for MRI findings, noting that 30-43% of OLTs visible on MRI are invisible on conventional radiography [121]. MRI can detect early biochemical changes before morphological damage appears.
→ Radiography = standard X-rays; morphological = visible structural changes
Advanced imaging techniques now allow quantitative assessment of cartilage quality [122]:
Raymond's lesion has been classified as Hepple Stage V (with cystic component), placing it in the most severe category.
→ Understanding normal = understanding how much damage exists. Talar cartilage is thin (about 1mm) - even small defects are significant.
MRI and cadaveric studies have established normal talar cartilage thickness values [123]:
→ Cadaveric = studied from deceased donors; gives true measurements without imaging distortion
Clinical significance: Smaller joints like the ankle have thinner cartilage, making MRI evaluation less accurate than in the knee.
→ Certain things make treatments less likely to work. Knowing these helps set realistic expectations and optimize conditions before surgery.
A 2025 study with minimum 5-year follow-up found [124]:
The 2024 JBJS 10-year survival study found [22]:
→ BMI = Body Mass Index, a weight-to-height ratio; ≥30 is considered obese
→ Wobbly ankle = damaged cartilage. Up to 70% of ankle sprains/fractures may cause OLT. Fixing instability protects cartilage repairs from failing.
Recent 2024-2025 studies reveal strong associations [126]:
Joint line tenderness lasting >6 weeks strongly predicts presence of OLT (p<0.001) [126]. Physical examination has low sensitivity for detecting OLT - MRI recommended for persistent symptoms.
→ Joint line tenderness = pain when pressing directly on the ankle joint; sensitivity = how well a test catches problems
A 2024-2025 study found [127]:
Clinical pearl: If you had significant ankle sprains before your OLT, addressing any residual instability is critical for long-term success of cartilage treatment.
→ "Conservative" means managing without surgery: rest, PT, bracing, anti-inflammatories. The cartilage won't heal, but symptoms may calm down.
The first prospective study assessing nonoperative treatment for OLTs was published in 2025 [13]:
→ Prospective study = follows patients forward in time (stronger evidence than looking backward)
A 2024 systematic review of 2,347 cases found [64]:
A 2025 systematic review on juvenile OLTs found [65]:
Best for: Non-displaced Grade I-II lesions, skeletally immature patients, patients with minimal symptoms. Patients who receive nonoperative management seldom recover to their previous level of sports activity [10].
→ HA is a gel-like lubricant naturally in joints. PRP uses your own blood's healing factors. Neither creates new cartilage, but they may reduce inflammation and pain.
A systematic review of 3 randomized controlled trials (132 patients) found HA injection as an adjunct to microfracture provides clinically important improvements [15]:
→ RCT = Randomized Controlled Trial (gold-standard study design); adjunct = added alongside another treatment
A 2024 meta-analysis from the Journal of Orthopaedic Surgery and Research (5 RCTs) found [67]:
→ SMD = Standardized Mean Difference; negative value = less pain (good); OA = osteoarthritis
A 2025 systematic review from Arthroscopy Journal found important safety data [68]:
A network meta-analysis of 6 RCTs (295 patients) compared adjuncts to microfracture [69]:
→ Network meta-analysis = combines multiple studies to compare treatments that may not have been directly compared
HA was FDA approved in 1997 for knee osteoarthritis only. FDA has not approved intra-articular HA for ankle joints, though it is commonly used off-label [17]. A 2024 CADTH rapid review confirmed limited evidence for ankle applications [70].
→ Intra-articular = injected into the joint; off-label = approved for another use but legally prescribed by doctors for this one
→ Microfracture pokes tiny holes in bone to cause bleeding. Stem cells from bone marrow form a clot that becomes "fibrocartilage" - scar-like tissue that's not as strong as real cartilage, but can reduce pain. Like patching with duct tape instead of the original material.
A 2025 systematic review of 43 studies (2,721 patients, 5-24 year follow-up) found [71]:
A 2025 study in Indian Journal of Orthopaedics reports 5-year outcomes [72]:
→ DGOU = German Society of Orthopedics and Traumatology (respected European guidelines)
A 2025 meta-analysis found no clinical difference between simple and cystic lesions if cyst depth <5-6mm, medial talus location, and patient <40 years old [26].
→ Cystic lesion = has a fluid-filled hole in the bone; simple = just cartilage damage without a bone cyst
However, for large cystic OLT (>300 mm³), autologous osteochondral transfer showed superior survival vs BMS (p=0.042) [27].
→ Autologous = using tissue from your own body (from another location)
Fibrocartilaginous repair tissue tends to degenerate over time. Good clinical outcomes at midterm, but radiological outcomes showed repair tissue surface damage [20]. This may be a harbinger for long-term problems [28].
→ Fibrocartilaginous = scar-like cartilage (weaker than original hyaline cartilage); harbinger = warning sign
→ BioCartilage and AMIC add a "helper layer" on top of microfracture. A scaffold (like a cartilage-protein sponge) gives healing cells a structure to grow on. Like providing scaffolding for construction workers instead of building in mid-air.
BioCartilage is dehydrated, micronized allogeneic cartilage containing extracellular matrix (type II collagen, proteoglycans, cartilaginous growth factors). It acts as a scaffold over microfractured defects [29].
→ Allogeneic = from a donor (not your own tissue); extracellular matrix = the "glue" between cells; proteoglycans = cushioning molecules in cartilage
A June 2024 systematic review of 15 studies (12 case series for meta-analysis) [31]:
→ AMIC = Autologous Matrix-Induced Chondrogenesis; combines microfracture with a collagen membrane
A 2025 study in Cartilage evaluated 10-year outcomes [73]:
Efrima et al. 2024 evaluated arthroscopic AMIC at 24 and 60 months [74]:
→ OATS takes a plug of healthy cartilage+bone from your knee and presses it into the ankle defect like a cork in a bottle. Your own tissue = no rejection risk. Downside: creates a new wound in your knee.
Systematic review with 10.2 year mean follow-up (610 patients, 10 studies) [35]:
A 2024 systematic review in JOSR evaluated OATS outcomes [75]:
Autografts significantly outperform allografts [38]:
→ Autograft = your own tissue; Allograft = donor tissue (like a transplant)
Recent advances in osteochondral autograft procedures [76]:
→ Donor site morbidity = problems caused at the site where tissue was taken (the knee, in OATS procedures)
Systematic review of 1726 patients (21 studies) [39]:
→ MCP = mosaicplasty (multiple small plugs); DSM = donor site morbidity
A 2025 study on predictors of donor site morbidity found [40]:
Emerging technique using autologous ipsilateral talus grafts [78]:
→ Ipsilateral = same side; taking cartilage from another part of the SAME ankle instead of the knee
Key issue: Patients receiving 2+ plug grafts have worse knee scores (96 vs 98, p<0.05). Knee and talus cartilage do not biomechanically match [39].
→ Uses cartilage+bone from a deceased donor (cadaver) instead of your own body. Like an organ transplant for cartilage. Advantage: no donor site pain. Downside: potential rejection, tissue isn't "alive" like yours.
A 2024 comprehensive review of fresh osteochondral allograft (OCA) outcomes [79]:
Recent 2025 data on fresh talar allografts [80]:
A 2024 comparative analysis evaluated bulk hemitalar vs shell allografts [81]:
Systematic review of 115 failed bulk allografts [44]:
New data on revision allograft surgery [82]:
Critical for Raymond: Allografts have 5-7x higher failure/revision rates vs autografts [38]. These procedures should be thought of as an intermediate step before fusion/replacement [45].
→ DeNovo uses tiny cartilage pieces from young donors (under 13). Young cartilage has more "stem cell-like" properties. Mixed with fibrin glue and placed into the defect.
Recent studies have provided more data on particulated juvenile cartilage [83]:
Long-term case report with second-look arthroscopy showed graft survival at 11 years [47].
DeNovo NT (natural tissue) is manufactured by Zimmer Biomet. Availability may be limited in some regions, and cost remains significant (~$5,000-8,000 for the graft alone) [84].
Conclusion: High complication and failure rates call into question efficacy for large OLTs. Cannot be currently recommended for lesions >125mm² [46].
→ Bone under cartilage has a hole (cyst) filled with fluid. Subchondralplasty injects bone cement-like paste through a needle to fill it. The paste hardens and becomes part of your bone. Like filling a pothole in a road.
Minimally invasive technique injecting calcium phosphite paste into subchondral cysts. The paste crystallizes like cancellous bone to fill the defect [48].
Recent studies have expanded understanding of this technique [85]:
A 2024 comparative study examined different bone substitutes [50]:
Alternative approach: retrograde drilling has ~90% success rate for intact cartilage lesions [52]. However, failure rates can reach 20% due to inaccurate targeting [53].
Newer navigation technologies improve accuracy [52]:
For Raymond: Dr. Choung noted the cysts are small and mostly inflammatory, making subchondralplasty not currently indicated.
→ ACI: Two surgeries. First, surgeon takes healthy cartilage cells and a lab grows millions more (4-6 weeks). Second surgery implants them. MACI grows cells on a scaffold membrane for easier implantation.
A landmark 2024 study evaluated first-generation ACI with minimum 20-year follow-up [90]:
A 2024 systematic review of 166 MACI patients [91]:
→ Experimental treatments using stem cells (from fat, bone marrow, etc.) to regenerate cartilage. Stem cells are "blank" cells that can become cartilage cells. Exosomes are tiny healing signal packets cells release.
The German Society of Orthopedics and Traumatology considers adipose-derived MSC therapy for OLT experimental [92]:
→ Adipose-derived = from fat tissue; MSC = Mesenchymal Stem Cells (cells that can become cartilage)
A November 2025 case using heparin-conjugated fibrin hydrogel with MSCs [93]:
→ Hydrogel = gel-like scaffold that holds cells in place; fibrin = natural clotting protein
Exosomes are emerging as potential therapy for cartilage repair [94]:
CBMA is a simpler stem cell approach harvested during surgery [1]:
→ CBMA = liquid from inside your bones (rich in stem cells) concentrated and applied to the defect
Status: These therapies show promise but remain largely experimental. No large RCTs yet for ankle OLT specifically.
→ High-energy sound waves (tiny sonic booms) directed at the damaged area. Stimulates healing by increasing blood flow and reducing inflammation. Non-invasive, done in office visits. Like jump-starting your body's healing response.
A July 2025 study evaluated combined therapy for OLT [95]:
A 2024 study in Bone & Joint Research [96]:
A 2023 study comparing MF+ESWT vs MF+PRP [97]:
OLT has been recognized as an indication for ESWT by the International Society for Medical Shockwave Treatment since 2008 [98].
Best for: Non-invasive adjunct therapy, especially combined with microfracture. Can reduce pain and improve outcomes without additional surgery.
→ PEMF devices generate low-frequency electromagnetic waves that penetrate tissue. Thought to stimulate cellular repair, reduce inflammation. Completely non-invasive - just place device near ankle daily. Like giving cells a gentle energy boost.
Recent studies show promising mechanisms for PEMF in cartilage repair [99]:
NASA Johnson Space Center developed a PEMF device showing that waveform variation influences genetic regulation of chondrocytes from early OA patients [102].
Status: Promising adjunctive therapy, but not a standalone treatment for OLT. Best as part of a comprehensive conservative management approach.
→ PT isn't just for after surgery - it's core treatment at every stage. Focuses on reducing pain, improving motion, strengthening muscles, and training ankle to move properly (proprioception).
A 2024 meta-analysis of 200+ studies found large variation in rehab protocols [103]:
Key elements of physical therapy for OLT [104]:
General rehab phases after cartilage surgery [105]:
A 2025 narrative review noted that high-quality studies on physical therapy for OLT remain relatively few [106]. However, preoperative assessment and postoperative functional rehabilitation are considered critical components of successful OLT management.
Key point: Finding a PT experienced with ankle cartilage injuries can make a significant difference in outcomes. Full recovery often takes up to 12 months.
→ When cartilage treatments fail: Fusion (arthrodesis) permanently joins ankle bones = eliminates pain AND motion. Replacement (arthroplasty) = artificial joint like hip/knee, preserves motion but needs eventual revision. Both are major surgeries with long recovery.
Recent studies show significant improvements in newer implant designs [86]:
Third-generation designs show improved results vs older prostheses. At medium-term, TAA is at least as effective in patients <50 as in older patients [59].
Recent national registry analyses provide large-scale outcome data [88]:
Newer fusion techniques show improved outcomes [89]:
For painful fusions, conversion to TAA is possible [62]:
Key point: All doctors agreed ankle fusion should be avoided for someone young with good ROM. Cleveland Clinic noted TAA would be a later escalation step.
→ Extra weight = more stress on ankle cartilage with every step. Obesity linked to worse surgical outcomes. Like driving on a weak tire - heavier load = faster wear. Weight management can significantly affect how well treatments work.
A 2025 study from the German Cartilage Registry (303 patients) examined BMI impact on OLT surgical outcomes [107]:
The 10-year survival study analyzed BMI as a risk factor for treatment failure [22]:
Takeaway: While not a contraindication to surgery, maintaining healthy weight optimizes outcomes.
→ Glucosamine, chondroitin, collagen = cartilage building blocks taken as pills/powders. Gives body extra raw materials. Research is mixed - may help pain modestly. Generally safe but unlikely to regenerate destroyed cartilage.
A comprehensive 2025 review of 146 studies on glucosamine and chondroitin [108]:
A 12-week randomized controlled trial (52 participants) on combination supplements [109]:
NIH/NCCIH notes mixed evidence [110]:
Bottom line: Generally safe to try for 3-6 months. May provide modest pain relief. Not a substitute for proper medical treatment.
→ Gene therapy = giving cells new instructions. Delivers genes that tell cells to produce more cartilage proteins. Still experimental for ankle - most research in lab animals - but represents the future of repair.
Gene therapy for cartilage is advancing but not yet clinically available for ankle OLT [112]:
A recycled cartilage auto/allo implantation technique is being studied [114]:
Status: Experimental. Not available for routine clinical use in 2025.
→ Getting back to sports is a long journey. Procedure type determines wait time. Simpler = faster return but less durable tissue. Complex = longer wait but better long-term tissue. Most return to some sports, but often modify activities.
Systematic review of 2,347 OLT cases [115]:
A 2024 study on OCA transplantation in athletes [118]:
For skeletally immature athletes with OLT [119]:
Important considerations from the literature:
→ To access OLT, surgeons sometimes need to temporarily cut the ankle bone (malleolus) and move it aside. Like opening a hatch to reach inside. It heals after, but adds recovery time and potential complications.
Posteromedial lesions are often difficult to access with arthroscopy alone and may require a medial malleolar osteotomy (MMO). The 2024 DGOU recommendations note that MMO has a minor effect on clinical outcome compared to other factors [128].
A large registry study examined MMO prevalence and consequences [129]:
A 2025 comparison study found [130]:
A 2025 study on adolescent athletes found 75% had osteotomy fixation screws removed due to hardware irritation [131]. Osseous union typically occurs at 6.2 weeks average.
→ When biological treatments fail, a metal cap can resurface the damaged area. Think of it like a dental crown for cartilage. It's a salvage option - a last-ditch effort before fusion/replacement.
Metal resurfacing was proposed for large osteochondral defects not successfully treated with other surgical treatments. The HemiCAP implant is available in 15 articular component offset sizes based on medial talar dome anatomy [132].
Implantation accuracy is crucial [133]:
Status: Salvage procedure for failed biological treatments. Not recommended as first-line option.
→ "Revision" = doing surgery again after a first surgery failed. Success rates are lower than first-time surgery. The more revisions, the harder it gets.
A systematic review found concerning outcomes for revision cases [21]:
When osteochondral autograft transplantation fails with concomitant malalignment [134]:
A study on repeat procedures found [135]:
Key point: Revision success rates are consistently lower than primary surgery. Prevention of initial failure through proper technique and patient selection is crucial.
→ Fresh allografts (from recently deceased donors) have living cells but limited shelf life. Cryopreserved (frozen) grafts last longer but cells may be dead. New tech is bridging this gap.
A 2025 study found promising results for cryopreserved grafts [136]:
Fresh allografts have been favored due to [137]:
→ Scientists are developing ways to 3D print cartilage and bone scaffolds custom-made for each patient's defect. Still experimental but represents the future of joint repair.
Researchers from Singapore and Manchester developed a layered scaffold that mimics natural bone and cartilage structure [139]:
PCL-based biphasic designs now offer [140]:
Status: Primarily laboratory research. Clinical translation ongoing. Represents promising future direction for complex OLT repair.
→ Your mental state affects surgical outcomes. Anxiety and depression are common with chronic pain. Addressing mental health can improve physical recovery.
A landmark 2024 study examined psychological status in OLT patients [141]:
A meta-analysis of 115,380 orthopedic patients found [142]:
Takeaway: Managing pain-related anxiety and depression is an important part of comprehensive OLT treatment.
→ PRF is like PRP but contains more of the healing factors and a fibrin scaffold. Simpler preparation, no additives needed. May provide longer-lasting effects than PRP.
A retrospective study of 15 patients with stage IV OLT found [143]:
A study combining PRP with AOT in patients with OLT + chronic lateral ankle instability found [144]:
PRF provides a natural fibrin-based biomaterial scaffold rich in platelets, growth factors, and cytokines that facilitates cellular migration and proliferation essential for tissue healing.
Based on the research, a reasonable progression might be:
All sources are peer-reviewed systematic reviews, meta-analyses, randomized controlled trials, or major clinical studies from 2016-2025. Emphasis on 2024-2025 publications.